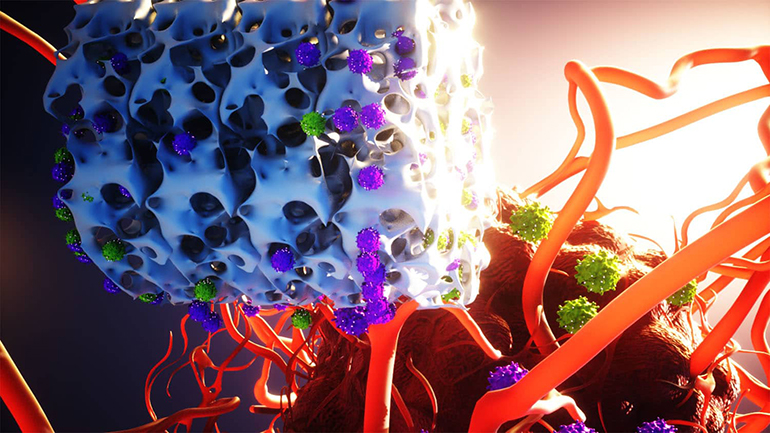
Researchers at North Carolina State University developed an implantable biomaterial scaffold that enables the creation and release of CAR-T cells, which are immune cells that have been engineered and primed to seek and destroy cancer within the body. The technique could prove to be much less expensive than conventional CAR-T cell therapy, and it may also be more effective if the early promising results in animals can be replicated in human patients. Classic CAR-T treatment involves weeks of laboratory cell work, which contributes to its high cost, whereas this new technique can be performed in just one day.
“A major drawback to CAR-T cell treatment is that it is tremendously expensive — hundreds of thousands of dollars per dose,” said Yevgeny Brudno, one of the creators of the new scaffold. “Due to its cost, many people are shut out from this treatment. One reason for the high cost is that the manufacturing process is complex, time-consuming, and has to be tailored to each cancer patient individually. We wanted to address challenges in CAR-T treatment related to both manufacturing time and cost.”
To generate CAR-T cells, typically clinicians will isolate T cells from a cancer patient and then activate them using antibodies and reprogram the cells through genetic modification using viral vectors. Finally, the clinicians encourage the cells to proliferate, and when they have enough, they can administer them into the patient’s bloodstream. This is an incredibly protracted and expensive process, taking weeks.
This new solution, which the NCSU researchers dubbed Multifunctional Alginate Scaffolds for T cell Engineering and Release (MASTER), aims to achieve cell reprogramming, proliferation, and release all within the body of the patient. “Our MASTER technology takes the cumbersome and time-consuming activation, reprogramming and expansion steps and performs them inside the patient,” said Pritha Agarwalla, another researcher involved in the study. “This transforms the multi-week process into a single-day procedure.”
In this new paradigm, clinicians would isolate T cells from a patient as normal, but instead of taking them away for reprogramming in a clean facility, they would mix them with a viral vector immediately, add them to an alginate biomaterial scaffold, and then implant it back into the patient’s body the same day. The MASTER implant is studded with antibodies that help to activate the T cells so that can occur straight away on the scaffold.
So far, the technology has proven to be more effective at fighting cancer in mice than conventional CAR-T cell treatments, suggesting that it has significant clinical potential. “The end result is that the mice that received CAR-T cell treatment via MASTER were far better at fighting off tumors than mice that received conventional CAR-T cell treatment,” said Agarwalla.
Study in Nature Biotechnology: Bioinstructive implantable scaffolds for rapid in vivo manufacture and release of CAR-T cells