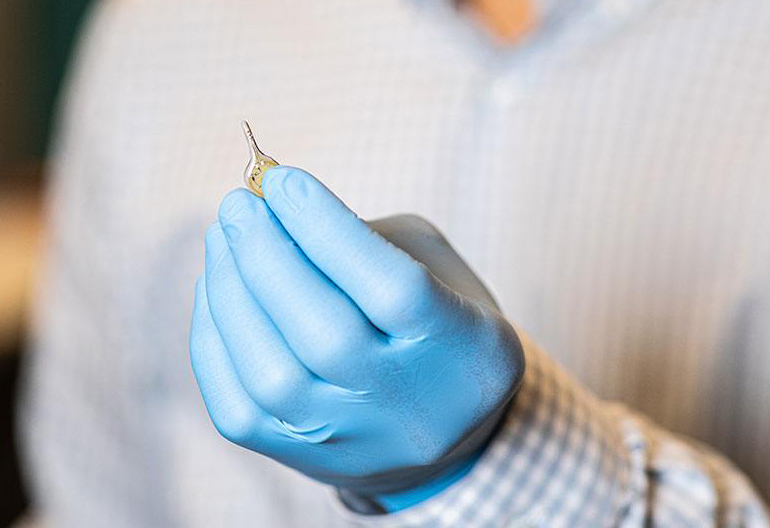
Researchers at Texas A&M University created a wireless device that aims to illuminate and destroy residual tumor cells left after cancer resection. The device can be used by surgeons to illuminate the tumor bed after resection. It works in combination with a photosensitizer drug that is administered before the procedure and accumulates in tumor cells, making them vulnerable to the lethal effects of the delivered light. The small device can also be implanted within the body, potentially to provide longer term photodynamic therapy and guard against cancer recurrence.
For many cancers, surgery is the primary treatment, followed by supplementary chemotherapy to kill any remaining cancer cells that were not removed by the surgeons. Chemotherapy entails pretty severe side-effects, and so a long-term goal for researchers involves finding gentler alternatives. Photodynamic therapy, where light in combination with a photosensitizer effectively kills cancer cells is one such option, but the technology has yet to gain significant traction.
Part of the problem lies in how little researchers know about the correct dose of light to use to appropriately affect cancer cells, and an inability to adjust the dose based on the tumor response. Moreover, wireless implantable technologies that allow for long-term therapy would be particularly beneficial in enhancing the clinical utility of the technique.
This technology aims to be a big step in the path towards enhancing the clinical potential of photodynamic therapy. “The biocompatible, miniaturized implantable LED device will enable light dosing and PDT that is tailored to the individual tumor response,” said Sung IL Park, a researcher involved in the study. “The intracavity device will provide a minimally invasive, biocompatible platform for light detection of residual cancers and delivery to tumor cells located in any part of the body, suggesting it could make an impact in the areas of breast, kidney, lung, pancreatic, prostate , ovarian and rare cancers.”
The device allows the researchers to tune the wavelength of light to precisely match the absorption spectrum of the photosensitizer drug, enhancing the efficacy of the technique. The small size and wireless nature of the technology allow it to be positioned optimally to affect residual cancer cells, and helps to avoid the poor tissue penetration issues of other photodynamic technologies.
The system also has low energy demands, making it efficient to run for extended periods. So far, the researchers have optimized the technology for use in experimental animals, so clinical translation will require further work.
Study in Nature Communications: AI-enabled, implantable, multichannel wireless telemetry for photodynamic therapy
Via: Texas A&M