Aafter 38 years as the head of the National Institute of Allergy and Infectious Diseases, dr Anthony Fauci announced on Monday that he will be stepping down from his role in December. Appointed to the position in 1984 by then-President Ronald Reagan, Fauci has personally overseen the federal government’s response to some of the 20th century’s deadliest infectious diseases — from tuberculosis and COVID to SARS and MERS.
But, as he told The Guardians in 2020, “my career and my identity has really been defined by HIV.” The prevention and treatment of HIV has been a prioritized area of research for the NIAID since 1986, and one that Dr. Fauci has devoted much of his public service to. The current state of AIDS research and response in America is thanks in no small part to his continued efforts in the field.
The NIAID is one of 27 specialized institutes and centers that make up the National Institutes of Health (NIH), which in turn reports to the Department of Health and Human Services. The NIH overall serves as the federal government’s premiere health research program. The NIAID operates within that bureaucratic framework, conducting and supporting “basic and applied research to better understand, treat, and ultimately prevent infectious, immunologic, and allergic diseases,” per its mission statement. That includes everything from working to mitigate effects of the annual influenza strain and alleviate asthma in urban youth to leading the development of an effective vaccine against COVID-19. The technology behind that vaccine is now being adapted for use against HIV and malaria as well.
Working at the forefront of immunoregulation research in the early 1980s, Fauci developed treatments for a class of otherwise-fatal inflammatory diseases including polyarteritis nodosa, granulomatosis with polyangiitis (formerly Wegener’s granulomatosis) and lymphomatoid granulomatosis. The results of those studies helped lay the groundwork for today’s research by the NIAID’s Laboratory of Immunoregulation. That research includes cellular and molecular mechanisms of HIV immunopathogenesis and the treatment of immune-mediated diseases. Combining the institute’s nearly four decades of HIV/AIDS research with cutting edge genomic technology has brought us not one, but three potentially viable AIDS vaccinesall of which are currently in clinical trials.
“Finding an HIV vaccine has proven to be a daunting scientific challenge,” Dr. Fauci said in a March NIAID release. “With the success of safe and highly effective COVID-19 vaccines, we have an exciting opportunity to learn whether mRNA technology can achieve similar results against HIV infection.”
The active, hands-on approach we see in response to the AIDS epidemic today is a far cry from that of the Reagan administration at the start of the crisis in 1983, which initially met the issue with silence. That is, outside of the time Larry Speakes, Reagan’s press secretarycalled it “the gay plague.”
Fauci’s initial efforts during the AIDS epidemic did more harm than good. In 1983, he published The Acquired Immune Deficiency Syndrome: The Ever-Broadening Clinical Spectrum in which he warned of “the possibility that routine close contact, as within a family household, can spread the disease.” We know now that this is not at all how HIV works, but at the time — despite the study urging caution until more evidence was gathered — it set off a moral panic in the media. The study was subsequently picked up by right-wing organizations and used as a political cudgel blaming the LGBTQIA+ community for the disease.
Reagan himself didn’t publicly mention the crisis until 1985, three years after it was officially identified by the CDC (and, coincidentally, a month after he admitted his involvement in the Iran-Contra Scandal). Social stigma around the disease made funding for basic health research nearly impossible to acquire, and was exacerbated by Reagan’s repeated budget cuts to the NIH and CDC.
“The inadequate funding to date has seriously restricted our work and has presumably deepened the invasion of this disease into the American population,” a CDC staffer wrote in an April, 1983 memo to then Assistant Director, Dr. Walter Dowdle. “In addition, the time wasted pursuing money from Washington has cast an air of despair over AIDS workers throughout the country.”
Even after his appointment as Chief Medical Officer — one who was determined to treat the AIDS crisis with its deserved gravity — Fauci faced pushback from the LGBTQIA+ communitywho demanded greater action from the government in response to the crisis and sought to accelerate the glacial pace of drug trials at the time.
By 1990, the community’s patience had reached a breaking point, resulting in ACT UP’s (AIDS Coalition to Unleash Power) attempt to storm the NIH in protest. “One of the things that people in ACT UP said is that we are the people who are experiencing this novel disease, and we are the experts, not just the scientists and doctors,” Garance Ruta, executive director of GEN magazine and an ACT UP member at the protest, told The Washington Post in 2020.
“I was trying to get them into all the planning meetings for the clinical trials,” Fauci told WaPo, in response. “I felt very strongly that we needed to get them into the planning process because they weren’t always right, but they had very, very good input.”
Over the last 30 years, the NIH has helped lead development of numerous antiretroviral therapies. azidothymidines (AZT), the first drug discovered to inhibit HIV’s replication without damaging cells, which was initially developed by the NIH as an anti-cancer drug in the 1960s. Its use as an antiretroviral, approved by the FDA in 1987, helped to establish the AIDS Clinical Trials Group (ACTG), which further accelerated research into nucleoside reverse transcriptase inhibitors (NRTIs, the class of drug to which AZT belongs). NIAID-funded studies in the 1990s helped establish combination therapies, which combine multiple medications for a synergistic effect, and explored a newly-identified class of drug, non-nucleoside reverse transcriptase inhibitors or NNRTIs.
NIAID
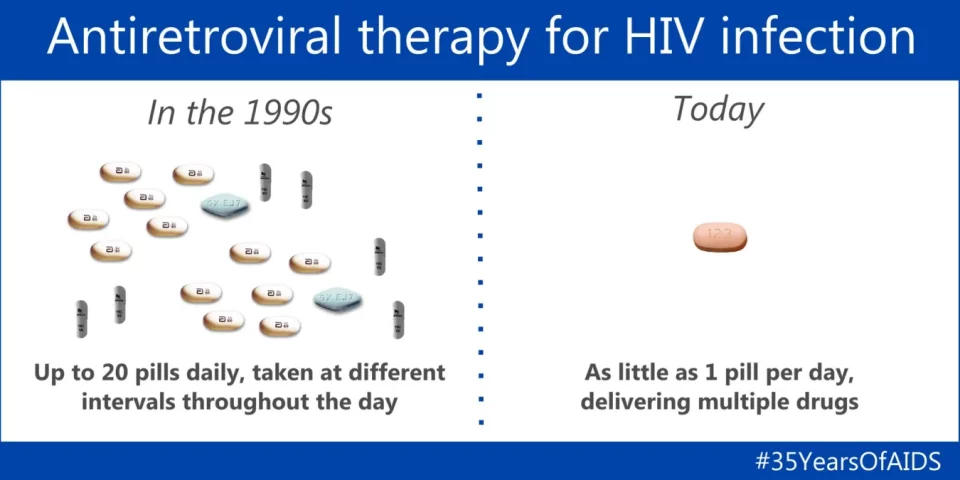
Today, nearly three dozen antiretroviral drugs are available, many of them combined into fixed-dose tablets. In the 1990s, people living with AIDS would be expected to take up to 20 individual pills at set schedules throughout the day. The average lifespan for someone infected with the disease was roughly a year. Today, assuming you’re lucky enough to live in the developed world, AIDS has become a chronic condition to be controlled with a single daily pill. For the 20 million people living with AIDS but without access to modern treatment, it remains a death sentence.
The state of medical research technology has also evolved, even if the nation’s prevailing notions of fairness and equality haven’t improved much in the intervening years since Reagan held power. Advances in laboratory standardization and automation have rapidly reduced development cycles and the occurrence of outlier results. The monotonous tasks that were once performed by lab assistants are now handled by robotic arms equipped with pipette arrays.
Disease prevention and diagnosis efforts have been augmented in recent years with artificial intelligence and machine learning algorithms. They’ve also found use in helping to stem the spread of HIV and improve access to both retrovirals and PReP with applications including, “ML with smartphone-collected and social media data to promote real-time HIV risk reduction, virtual reality tools to facilitate HIV serostatus disclosure, and chatbots for HIV education,” argue Drs Julia Marcus and Whitney Sewellof Harvard and UMass Amherst, respectively.
And just as Dr Fauci is, quite specifically, not retiring — “I want to use what I have learned as NIAID Director to continue to advance science and public health and to inspire and mentor the next generation of scientific leaders as they help prepare the world to face future infectious disease threats,” he noted in Monday’s announcement — the work of the NIAID is far from complete. Even as we slowly conquer existing scourges like COVID and HIV, re-emerging threats like monkey pox (Not to mention ancient killers like polio) will continue to appear on our quickly warming planet.
All products recommended by Engadget are selected by our editorial team, independent of our parent company. Some of our stories include affiliate links. If you buy something through one of these links, we may earn an affiliate commission.