Productivity improvements have helped a wide range of industries—except the health care industry. From 1999 to 2014, productivity in the health care sector increased by just 8%, whereas other industries achieved far greater efficiency gains of 18%. While productivity comparisons between industries tend to be inaccurate, they do show health care lags far behind other industries in terms of productivity and potential.
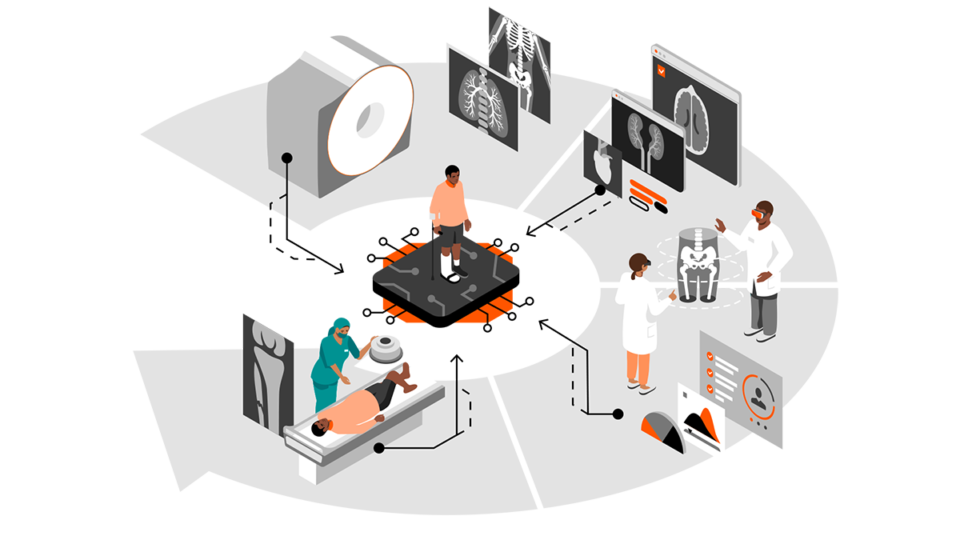
To operationally improve productivity in health care, two things must happen. First, data must be understood as a strategic asset. Data must be leveraged through intelligent and all-encompassing workflow solutions, as well as the use of artificial intelligence (AI)—driving automation and putting the patient at the center of the imaging value chain.
Second, to be able to speak of a value chain at all, the fields of competencies must be connected. The connection must be as seamless, open, and secure as possible. The goal is to ensure that all relevant data is available when needed by patients, health care professionals, and medical researchers alike.
A modern enterprise imaging software solution must prioritize outcome optimization, improved diagnostics, and enhanced collaboration.
Health care today: gaps, bottlenecks, silos
The costs and consequences of the current fragmented state of health care data are far-reaching: operational inefficiencies and unnecessary duplication, treatment errors, and missed opportunities for basic research. Recent medical literature is filled with examples of missed opportunities—and patients put at risk because of a lack of data sharing.
More than four million Medicare patients are discharged to skilled nursing facilities (SNFs) every year. Most of them are elderly patients with complex conditions, and the transition can be hazardous. According to a 2019 study published in the American Journal of Managed Care, one of the main reasons patients fare poorly during this transition is a lack of health data sharing—including missing, delayed, or difficult-to-use information—between hospitals and SNFs. “Weak transitional care practices between hospitals and SNFs compromise quality and safety outcomes for this population,” researchers noted.
Even within hospitals, data sharing remains a major problem. A 2019 American Hospital Association study published in the journal Healthcare analyzed interoperability functions that are part of the Promote Interoperability program, administered by the US Centers for Medicare & Medicaid Services (CMS) and adopted by qualifying US hospitals. The study showed that among 2,781 non-federal, acute-care hospitals, only 16.7% had adopted all six core functionalities required to meet the program’s Stage 3 certified electronic health record technology (CEHRT) objectives. Data interoperability in healthcare is not a matter of course.
Data silos and incompatible data sets remain another roadblock. In a 2019 article in the journal JCO Clinical Cancer Informatics, researchers analyzed data from the Cancer Imaging Archive (TCIA), looking specifically at nine lung and brain research data sets containing 659 data fields in order to understand what would be required to harmonize data for cross-study access. The effort took more than 329 hours over six months, simply to identify 41 overlapping data fields in three or more files, and to harmonize 31 of them.