Researchers at Johns Hopkins created an injectable hydrogel carrier vehicle for stem cells that is intended to aid in healing a difficult complication of Crohn’s disease, perianal fistulas. Perianal fistulas are very challenging to treat, but stem cells have shown promise in assisting with this process. However, it is difficult to get the cells to remain in place. This hydrogel delivery vehicle acts as a robust cell depot when injected near a fistula, keeping the cells alive and in place so that they can positively affect the healing process. The technology has shown promise in a rat model of Crohn’s-associated perianal fistulas.
Approximately 30-40% of Crohn’s patients will develop perianal fistulas. These consist of an inflamed tunnel between the body’s surface and the anal interior that can sometimes form as a result of a perianal abscess. The structures are painful and inconvenient, can become swollen and can leak blood or pus. This is one area of the body where no one needs an extra hole.
Surgery is often required, but over half of patients do not see any major benefit from current treatment approaches. “A large number of patients are diagnosed with Crohn’s disease in their late teens to early 20s, and they are contemplating a lifetime of suffering from perianal fistulas,” said Florin Selaru, a researcher involved in the study. “This condition in Crohn’s patients is notoriously difficult to treat. We hope these results offer a potential new treatment paradigm to be translated and to improve the quality of life for these patients.”
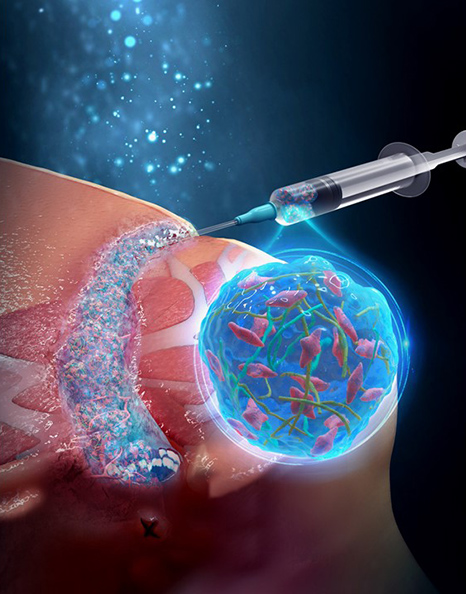
Stem cell injections have been shown to provide some healing efficacy in clinical trials when injected into or around the fistula tract. However, as with many cell therapies, keeping the cells alive and present in the target tissue is a challenge. Simply injecting a cell suspension directly into tissue is a very poor way to address this, and so researchers are developing a bewildering array of biomaterial carrier vehicles that can protect and retain cells.
The researchers used their gel to deliver adipose-derived stem cells in a rat model of Crohn’s associated perianal fistulas. The gel itself contained nanofiber fragments that are intended to create sufficient mechanical strength so that the cells are retained in place, regardless of the mechanical deformation of the gel bolus in the tissue.
The gel treatment reduced the size of the fistula tract by six-fold compared with surgical treatment, suggesting that the technology has significant potential as a treatment for perianal fistulas. “Think of it as a local delivery of a tissue regeneration nanogel-nanofiber composite that also keeps the stem cells at the site of the injury and enables the healing to occur,” said Selaru.
Studies in Science Advances: A nanofiber-hydrogel composite improves tissue repair in a rat model of Crohn’s disease perianal fistulas